SUMMARY
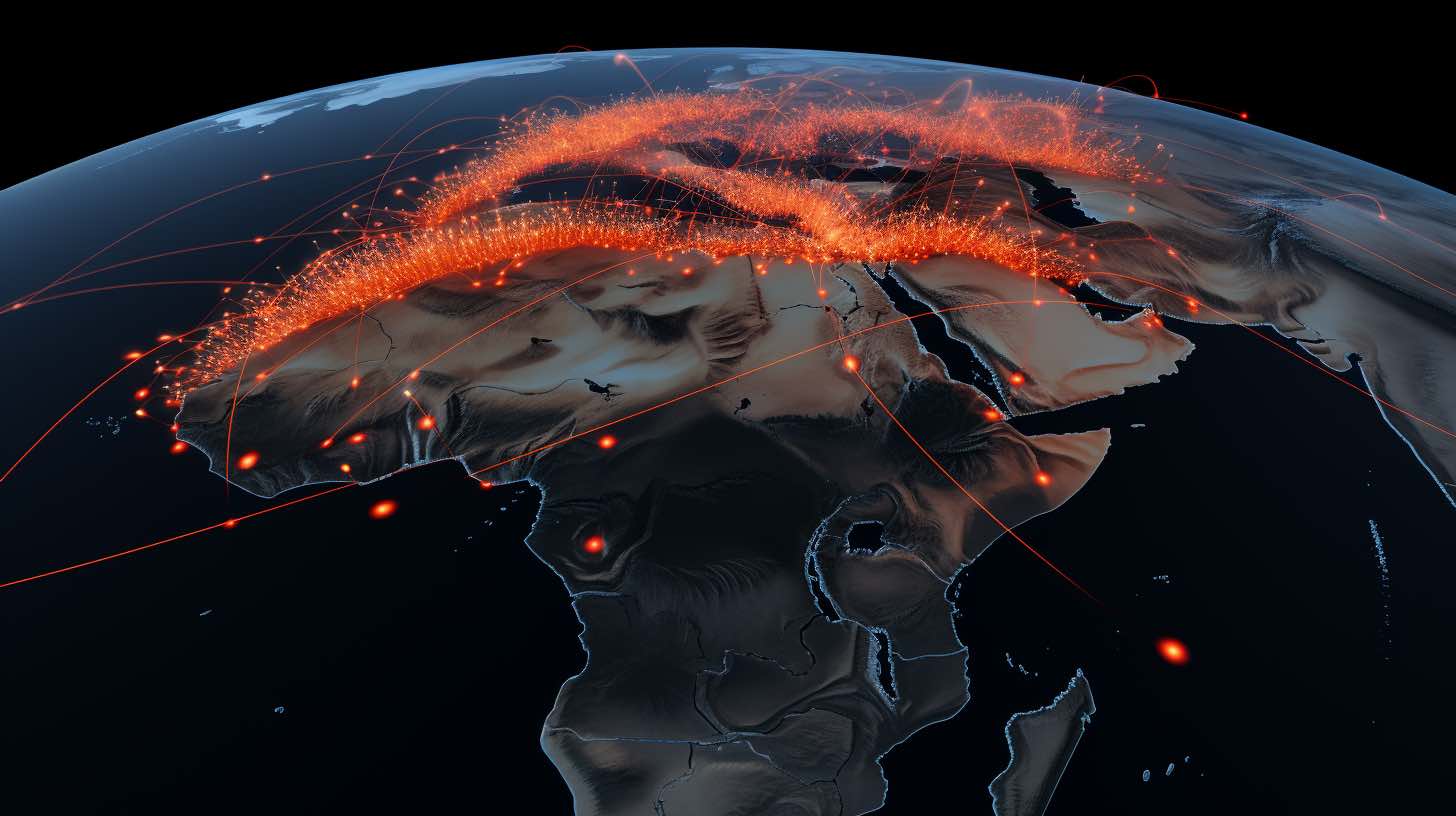
Recurrent disease outbreaks caused by a range of emerging and resurging pathogens over the past decade reveal major gaps in public health preparedness, detection, and response systems in Africa. Underlying causes of recurrent disease outbreaks include inadequacies in the detection of new infectious disease outbreaks in the community, in rapid pathogen identification, and in proactive surveillance systems. In sub-Saharan Africa, where 70% of zoonotic outbreaks occur, there remains the perennial risk of outbreaks of new or re-emerging pathogens for which no vaccines or treatments are available. As the Ebola virus disease, COVID-19, and mpox (formerly known as monkeypox) outbreaks highlight, a major paradigm shift is required to establish an effective infrastructure and common frameworks for preparedness and to prompt national and regional public health responses to mitigate the effects of future pandemics in Africa.
The colliding epidemics of Ebola virus disease, COVID-19, measles, and mpox (formerly known as monkeypox) outbreaks1 have highlighted inadequacies of current infrastructure and capacities for epidemic preparedness in Africa. The inequities of resource allocation and vaccine distribution during the COVID-19 pandemic have emphasised the need for Africa to advance its detection and response capacities.2 Capacity building in public health preparedness requires training and retaining public health experts. Building local ownership of health systems will help to improve the resilience of countries’ health systems during times of crisis, while contributing to improved health globally by reducing the risk of regional and global disease spread. National governments need to provide public health officials with sufficient legal authority with continuous and stable funding by leveraging the commendable efforts of the Africa Centres for Disease Control and Prevention (Africa CDC), to improve response to emerging and re-emerging pathogens in Africa.3
During the COVID-19 pandemic, global supply chains were severely disrupted. Contentious trade agreements and hoarding of supplies by resource-rich governments exacerbated shortages of essential items, especially in low-income and middle-income countries. National, regional, and global supply chains should be established to ensure equitable access to crucial supplies between and during crises. Supply chains should be decentralised to promote fair allocation of resources and maintain essential health system functions. Contracts should be established with suppliers of key commodities to procure essential supplies in a timely manner.2 Finally, local, and regional manufacturing and distribution capacities should be strengthened to improve production, as access to raw materials and transportation networks might be compromised during emergencies. During the COVID-19 pandemic, many factories in Africa switched to the making of essential supplies, and new partnerships were developed to improve manufacturing capacities. Manufacturers should be encouraged to increase their production capacity to respond to global health demands. National governments should establish partnerships with the private sector to build on the lessons learned from the Ebola virus disease and COVID-19 outbreaks.2
The time between the discovery of a new or re-emerging pathogen and its spread into a localised epidemic is a crucial window to prevent pandemics. Strong surveillance systems are essential for early detection, and the creation of data science hubs across Africa can support these efforts.4 These systems will require implementing public health laws for mandatory data reporting in electronic formats, and a stable information technology infrastructure with strong cybersecurity and confidentiality systems.4
Government agencies should cooperate to establish data science hubs staffed by scientists who will compile and analyse data in real-time, with high levels of completeness and accuracy. To support these hubs, Africa CDC, in collaboration with governments, will need to expand its multidisciplinary teams of disease detectives. High-risk zones might be identified with existing knowledge of disease burden, local epidemiology, and analyses performed at the hubs. Moving forward with a One Health approach, networks of local and regional multidisciplinary teams should consist of experts in human, animal, and environmental health to detect emerging pathogens with outbreak and pandemic potential.5
Field teams can report community-level data to the regional network in real time to support population-level analyses conducted at data science hubs.6 Access to diagnostics is essential to ensure that surveillance data are accurate. During the COVID-19 response, inadequate diagnostic capacity meant that health systems could neither detect nor predict true case numbers. Even when diagnostic tests are available, laboratories are often centralised and use tests that require advanced training, expertise, sample transportation processes, and infrastructure, leading to delayed results, especially in remote areas. There is a crucial need to establish local laboratory networks with robust systems for specimen transport, and for the return of test results via electronic data transmission to public health agencies using modern messaging methods. Recent efforts to leverage existing laboratory infrastructure for COVID-19 (eg, WHO Africa network of polio laboratories or HIV and tuberculosis GeneXpert PCR diagnostic capacity used for COVID-19 testing) at referral and university-level laboratories for decentralisation to community-level government laboratories, were commendable efforts and should be expanded. Furthermore, regional and national laboratories should have the ability to perform genomic sequencing to monitor new outbreaks and variants of concern. This capacity has been crucial throughout the COVID-19 response. The discovery of the omicron variant of SARS-CoV-2 by researchers in Botswana and South Africa in November, 2021, and the rapid sharing of data with international colleagues serve as examples of the global benefits of adequate diagnostic capacity in low-income and middle-income countries.7, 8
High-quality clinical trial infrastructure should be strengthened in Africa to provide regionally generalisable data, and ensure that therapeutics and vaccines are evaluated even if a disease is not prevalent in high-income settings. The ability to quickly identify or develop effective vaccines and treatments, including testing products off-label, will lead to more efficient containment of outbreaks. Multidisciplinary teams should be developed to conduct priority research at short notice during outbreaks. Robust and flexible platform trial methods and adaptive therapeutic trials9, 10 that were developed during Ebola virus disease outbreaks and the COVID-19 pandemic can be leveraged for new outbreaks and pathogens. Prompt regulatory review during these emergencies can also be adapted to promote greater efficiency in clinical research.
Trust should be developed before, during, and after outbreaks, and should build on honesty, transparent communication, and good governance—both by training public health experts in communicating effectively to counter misinformation and engage communities and their trusted leaders, including health-care workers, ministries of health, and religious and civil society organisations. During the Ebola virus disease response, community engagement and trust were interdependent and promoted safe burial practices, hand washing, and case identification.11 Similarly, during the COVID-19 pandemic, community cooperation was an essential part of containment efforts, bolstered by effective communication and leadership. Public health community advisory boards should be established and include trusted community leaders who can be consulted during health emergencies. Community advisory boards serve as important links between communities and health systems, filling the gaps in outreach activities and addressing misinformation, while ensuring that interventions are culturally appropriate and locally relevant. 11
Strong leadership, partnerships, and cooperation between scientists, clinicians, public health experts, health-care workers, government leaders, and funders are essential for outbreak control. Enhanced frameworks for global public health financing and accountability should be revisited and strengthened, building on the new World Bank Fund for Pandemic Prevention, Preparedness and Response, which promises to bring additional resources, incentivise country investment, and enhance partner coordination.12 However, in the context of competition for resources, as with the COVID-19 pandemic, national budgets should account for public health preparedness, and African countries should be as self-sufficient as possible, contributing to the local discovery and production of tools needed for responding to health threats.5
In summary, the COVID-19 pandemic revealed numerous gaps in global health preparedness and financing, highlighting the need for a paradigm shift towards a surveillance–response approach. Although the COVID-19 pandemic brought innovations, including improved surveillance, diagnostics, contact tracing, vaccine development, and treatments, enabling rapid identification of new virus variants and reduced morbidity and mortality, the benefits of these advances were inequitably distributed, and were limited by insufficient and delayed access in African countries. As a roadmap for African governments, stakeholders, and public–private health agencies to prepare for future pandemics, we call for: (1) strengthening public health preparedness, regional coordination, and response; (2) building supply chains for essential health supplies, including diagnostics, treatments, and vaccines; (3) establishing strong, integrated surveillance systems and monitoring using real-time data sharing and storage hubs with innovative digital tools; (4) decentralising and strengthening diagnostic laboratory capacity for diagnostics and pathogen genomics; (5) developing a robust clinical trial capacity; and (6) supporting community engagement and trust with a commitment to public health, leadership, coordination, and financing (panel). Finally, these improvements should be linked to well resourced and robust health systems and research networks that are prepared to address new health threats and translate early detection into rapid information sharing with coordinated health system responses in Africa.